Long COVID involves a wide range of symptoms and conditions that can last for weeks, months or even longer. In many cases it can have some quite debilitating effects. In this article we will look into some possible mechanisms where long COVID could come from, and what we can do to treat naturally the multiplicity of symptoms it can cause in our body.

A symptom is considered to be Long COVID if it lasts for more than 4 weeks after the illness has passed. Long COVID is more common among those who had a severe COVID-19 infection, but it can occur even among those who had an asymptomatic infection. The risk seems to increase also with age, and is less common in children and adolescents than in adults. Symptoms seem to be more common in women as well. There are more than 200 different symptoms listed in various studies. The more common ones include:
- extreme fatigue or tiredness that interferes with daily life
- shortness of breath, heart palpitations, chest pain or tightness
- cough
- hoarse voice
- difficulties with memory and concentration (brain fog)
- changes to taste and smell
- joint and muscle pain
- problems sleeping
- numbness or pins and needles
- changes in mood (anxiety, depression or stress)
- heart pounding or racing or heart palpitations
- joint pain
- muscle pain
- headache
- rash
- low-grade fever
- nausea and vomiting
- hair loss and skin changes
- reduced appetite and weight loss
- dizziness when standing up (lightheadedness)1)Understanding post-COVID-19 symptoms and long COVID https://www.healthdirect.gov.au/covid-19/post-covid-symptoms-long-covid
Long COVID or Post-COVID Conditions https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html
Fatigue is the most common post COVID symptom. Some studies show the close parallel between long COVID and chronic fatigue symptom, which is getting triggered by some kind of viral infections. This symptom is being studied for a while, but not much advance was made in viable treatment options. Because of the similarities, research in this condition called myalgic encephalomyelitis/chronic fatigue syndrome, or shortened as ME/CFS is giving some clues about possible mechanisms and treatment options of long COVID.
There is still much uncertainty what is causing long COVID. Some aspects can be explained by the damage of the proper virus. We know that even the isolated spike protein of the virus can cause organ damage. Others think that the infection is putting the immune system in overdrive, meaning that it attacks not only the virus, but the proper organs of the body. One study found unusually low cortisol levels and unusual activities of the immune system, that could point to a resurging dormant infection, for example Epstein Barr virus.2)Klein J. et.al. Distinguishing features of Long COVID identified through immune profiling https://doi.org/10.1101/2022.08.09.22278592

There is also no clearcut data of the prevalence of long Covid. One study showed 50.2% of positive COVID-19 cases to develop long COVID symptoms.3)Miranda D. et.al. Long COVID-19 syndrome: a 14-months longitudinal study during the two first epidemic peaks in Southeast Brazil. Transactions of The Royal Society of Tropical Medicine and Hygiene, Volume 116, Issue 11, November 2022, Pages 1007–1014, https://doi.org/10.1093/trstmh/trac030 That applied though to the first wave of the original virus and among patients that were sick enough to look for care at the emergency room of the hospital. In the US about 16 million people in the working age have some form of long COVID, and 2 to 4 million of those are estimated to be unable to work because of long COVID symptoms.4)Bach K. New data shows long Covid is keeping as many as 4 million people out of work. https://www.brookings.edu/research/new-data-shows-long-covid-is-keeping-as-many-as-4-million-people-out-of-work/ In the UK it is estimated that 2.1 million people, which is 3.2% of the population, has developed some form of long COVID symptoms.5) Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK: 3 November 2022 https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/3november2022
It is possible to develop the same kind of symptoms from the vaccine.6)So hoch ist Ihr Long-Covid-Risiko, wenn Sie sich jetzt infizieren Focus 31.10.2022 Considering that the vaccine produces a large number of spike proteins, and the immune system may overreact in some way, post vaccine effects are totally explainable. Symptoms are as diverse as for long COVID and can appear hours after vaccination, or take some days or weeks to develop. There are no statistics about the prevalence of those effects, (and probably won’t be for a while for political reasons) but most likely there are less prevalent then post COVID symptoms.
Possible Long COVID Mechanisms
The exact mechanisms of the long COVID are still not fully understood. There are several theories, but clear proofs are still missing.
One theory considers the possibility of the virus lingering in various tissues of the body. We know that the virus infects various organs in the entire body and can continue its activity long after respiratory symptoms have cleared. A study showed that 12% of COVID-19 patients were still showing up viral DNA in fecal PCR tests even 4 months after infection, and some 4% even after 7 months.7)Natarajan A, et.al. Gastrointestinal symptoms and fecal shedding of SARS-CoV-2 RNA suggest prolonged gastrointestinal infection. Med (N Y). 2022 Jun 10;3(6):371-387.e9. doi: 10.1016/j.medj.2022.04.001.
In order to prove the existence of live virus, tissue samples of the organs need to be drawn, which is a complicated invasive procedure and makes this theory hard to prove. For that reason, we still have no clear evidence whether the symptoms are caused by an inflammatory response after the disease, by organ damage that the virus has caused or by a still active virus in certain organ tissues. It may be even a combination of several factors, we just have no definite answers to that.
One argument in favor of the active virus theory are some isolated cases of patients that improved after being prescribed a series of antiviral medications, but there would be a need of randomized controlled trials to be able to generalize the efficacy of such therapy.
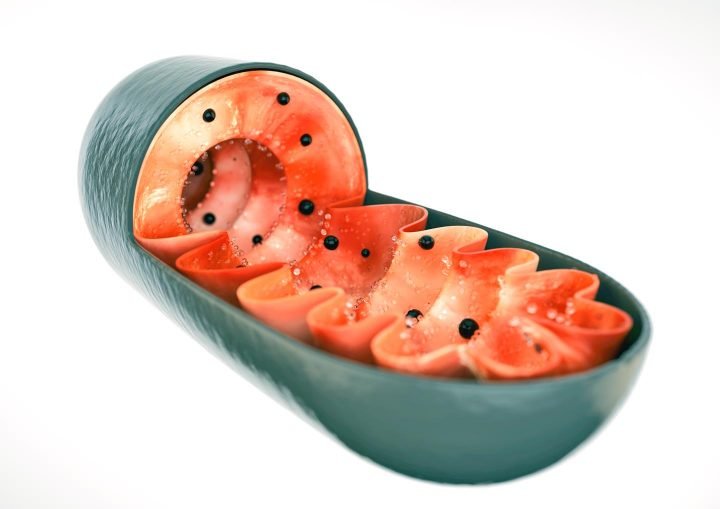
Inflammation seems to be another major component of the equation. COVID-19 uses the ACE-2 enzyme to enter the cell, an enzyme that is important to regulate inflammation. Lack of ACE-2 will increase inflammation, compromise the mitochondria, which is responsible for energy production and cause a number of other problems. The great number of ACE-2 receptors in the intestine are able to trigger gut dysbiosis.8)Mo Perry. How to Treat Long-Haul COVID. Experience Life
An overreactive immune system will also increase cytokine levels, which are the particles that the immune system uses to create inflammation and fight the virus. The SARS-Cov2 virus is able to damage the blood brain barrier, and cytokines will enter the brain, where they will affect major regulatory centers. They can affect the hypothalamus, responsible for hormone production (including for appetite and sleep control) and the autonomous nervous system, responsible for regulating heart rate, blood pressure and other important parameters. Obviously, this will affect fatigue in a significant way.
Inflammation caused by an immune system reaction to the remainders of the virus is also causing blood clotting to occur. This can limit blood flow to the muscles and be a possible cause for fatigue, pain and brain fog, among other symptoms. Inflammatory blood markers like D-Dimers among others can give a clue about inflammation going on after a viral infection.9)Shaffer L. Lots of long COVID treatment leads, but few are proven. https://doi.org/10.1073/pnas.2213524119
According to Etheresia Pretorius, a professor at Stellenbosch University in South Africa, the blood clotting is due to the spike protein of the virus. In a small trial she used a combination of 3 medications to control inflammation and normalize platelet activities, which resolved symptoms of fatigue and brain fog.10)E Pretorius , Combined triple treatment of fibrin amyloid microclots and platelet pathology in individuals with Long COVID/Post-Acute Sequelae of COVID-19 (PASC) can resolve their persistent symptoms. https://doi.org/10.21203/rs.3.rs-1205453/v1
Mast cells are regulating cells of the immune system that have a variety of different functions. They are commonly found beneath the skin, in the lungs and the digestive tract, and are constantly watching for invaders. In contact with certain allergens, they can overreact and cause inflammation, which is a major component of many allergic reactions. This mechanism possibly kicks in at Long COVID as well.
There is a disease called mast cell activation syndrome, when the allergic reaction is activated by a number of different triggers and difficult to control. A study showed that Long COVID had very similar symptoms to the mast cell activation syndrome, which could be another possible cause of Long COVID symptoms.11)Weinstock LB, et.al. Mast cell activation symptoms are prevalent in Long-COVID. Int J Infect Dis. 2021 Nov;112:217-226 doi: 10.1016/j.ijid.2021.09.043 High levels of tryptase, histamine, or prostaglandins in the blood may be an indicator of overreacting mast cells. Besides mast cell activation, other autoimmune mechanisms are considered as a possible cause.
In addition to circulatory problems, oxygen reaching a cell may not be able to produce sufficient energy due to compromised function of the mitochondria. It was observed that the SARS-CoV-2 virus can hijack the cell mitochondria, which are responsible for energy production. In the closely related chronic fatigue syndrome, compromised mitochondria are observed as well. We will discuss several supplements that can be useful in treating this condition.12)Astin R. et.al. Long COVID: mechanisms, risk factors and recovery. https://doi.org/10.1113/EP090802
Several researchers are looking how Long COVID is affecting the vagus nerve and causing a dysregulation of the sympathetic and parasympathetic nervous system. This can lead to fatigue, dizziness, heart palpitations and digestive problems. Noninvasive vagus nerve stimulation helped to decrease fatigue.
There are therefore a number of mechanisms that may be involved in producing Long COVID symptoms. Many of them are still hypothetical, but probably several of them are involved in producing the variety of symptoms classified as Long COVID. There may be even different mechanisms involved in every patient, which makes treatment still a lot of a trial-and-error endeavor. What works for one, may not work equally in another case.
Long COVID Treatment Options
Although all the mechanisms are not fully understood, a Long COVID treatment protocol should include:
- Reducing the inflammatory response and the resulting blood clotting.
- Strengthening the immune system and using substances with antiviral properties to eliminate possible remaining viral pockets.
- Assist the body in the process of mitochondria and cell repair.
- Give support to the nervous system.
Anti-inflammatory Diet
A healthy diet can go a long way to reduce inflammation, strengthen the immune system, nourish the cells and support the mind. A whole food plant-based diet will create the ideal conditions for that. Even if you are not willing to make a radical step to go vegan, you should consider to drastically reduce the quantity of animal products you consume, which tend to be high in cholesterol, saturated fats, arachidonic acid which promotes inflammation, unfavorable amino acid patterns, and a number of contaminants, causing a number of problems in the body, especially in the case of long COVID.
Omega 3 is a fatty acid with powerful anti-inflammatory properties. Doctors and Nutritionists often recommend fish as an Omega 3 source. Just, the beneficial effect of omega 3 is anilliated by saturated fats, cholesterol, mercury and other contaminants. Fish will fare well compared to red meat, but if you want to do something really good for your health, you should opt for plant sources of omega 3.
Good omega 3 sources are flaxseed, chia, hemp seed, walnuts, pumpkin seeds, Brussel sprouts as well as other cruciferous vegetables. All plant sources of omega 3 contain ALA, which needs to be transformed into the active forms DHA and EPA. EPA is known for its anti-inflammatory properties and benefiting the circulation, and DHA has some added benefits for the brain and the immune system. Under normal conditions, the body is able to transform sufficient ALA into its active forms, but in some conditions like long COVID, additional supplementation of the active forms may be warranted.

The most common source of DHA and EPA is fish oil. Again, we have the problem with contaminants. If you opt for fish oil, you should choose a brand that has IFOS certification, which includes testing for acceptable contaminant levels. The safer option would be to use vegan omega 3 supplements based on algae, which have much less contamination problems. After all, fish is getting their omega 3 from eating algae. A good dose for Long COVID treatment would be 4,000 mg daily of DHA & EPA combined.
While Omega 3 is quite essential, and the often abundant Omega 6 cause inflammation and needs to be reduced, care should be taken about the overall fat content. Excessive fat can influence negatively the microbiome of the intestine, which is having a negative impact on the immune system. Excessive fat can also contribute to obesity, which can increase inflammation and has a negative impact on immunity.
The same care should be taken to avoid any form of concentrated sugar in your diet. Sugar is very detrimental to the immune system, and on top of that is causing inflammation and increasing the perception of pain. Make a try if you can benefit from a complete elimination of all forms of concentrated sugar, including brown sugar, molasses, agave and maple syrup. Avoid artificial sweetener as well. Permitted are 1-2 tablespoons of honey a day and a moderate amount of dried fruits.

Another important component of an anti-inflammatory diet are antioxidants. They are constantly working to hold free radicals in check, and by avoiding the cell damage that free radicals would cause, they are reducing inflammation inside the body. The most popular ones are vitamin C, vitamin E, beta carotene together with minerals like selenium and manganese. The list goes on with innumerous other substances like glutathione, coenzyme Q10, flavonoids, polyphenols, phytoestrogens and many more. To get a good variety, it is recommended to eat a rainbow of fruits and vegetables every week. Antioxidants will help you quite a bit in treating brain fog, as well as increasing your energy levels.

Tumeric is a commonly used spice containing curcumin as an important anti-inflammatory active ingredient. It can inhibit the pro-inflammatory cytokines and has shown to have antiviral properties. You should make frequent use of this spice to benefit from its antioxidant properties.
There are a number of food items that will increase inflammation and should be avoided as much as possible. Those include:
- Sugar in all of its forms (including brown sugar)
- Extracted Oils high in omega 6
- Fried foods
- Saturated fat
- Cured meats
- Alcohol
- Caffeine
Supplements
It may be beneficial to supplement certain specific substances to help with recuperating long COVID. When supplementing, we need though proceed with caution. Not always are higher doses of a good thing providing a better result. Observing the right dosage is essential. And even so, often we have limited proof of its efficacy. Large scale randomized controlled trials would be needed to prove the efficacy of any kind of supplementation, and especially for long COVID we do not have such kind of studies available.
There are many cases that a natural fruit that is high in antioxidants is far superior to an isolated supplement. Inside of natural food sources, we have an intricate interplay between different phytochemicals, that we still not fully understand in all its complexity. An isolated substance rarely gives the same kind of benefits. If you opt for supplementing, you should wherever possible combine the supplement with natural food sources in order to maximize its benefits. Certain supplements are even produced out of dried fruits and vegetables and can often show superior results compared to synthetically produced supplements.
Even though we have very little data specifically to long COVID, there is one small scale study that prescribed a daily supplement of Vitamin C, acetyl L-carnitine, olive poliphenols, thiamine, vitamin B6, folic acid, vitamin D and vitamin B12. They reported a doubling of energy during the 2-week study period. This preliminary findings are very positive.13)Naureen Z et.al. Proposal of a food supplement for the management of post-COVID syndrome. European Review for Medical and Pharmacological Sciences, 2021; 25 (1 Suppl): 67-73
N-Acetyl-L-Cysteine (NAC) is an amino acid that can help in the production of glutathione, which in turn is a powerful antioxidant, especially protecting the mitochondria. It is also helping to strengthen the immune system. Avocado, okra, spinach, squash, melons, peaches and cruciferous vegetables (broccoli, cauliflower, cabbage and kale) can all help to increase glutathione levels. In case of Long COVID, NAC can give a very helpful boost for glutathione activity. Try to supplement with 600-1500 mg/day.
Resveratrol is an antioxidant found in red grapes, the skin of peanuts and some berries. It has specific protective function in case of COVID-19 infection and the resulting inflammation. Long COVID patients can benefit by supplementing with 200mg to 500mg of Resveratrol twice daily.14)Moriya J, Chen R, Yamakawa J, Sasaki K, Ishigaki Y, Takahashi T. Resveratrol improves hippocampal atrophy in chronic fatigue mice by enhancing neurogenesis and inhibiting apoptosis of granular cells. Biol Pharm Bull. 2011;34(3):354-9. DOI: 10.1248/bpb.34.354
Mo Perry. How to Treat Long-Haul COVID. Experience Life Resveratrol has often limited bioavailability.15)Walle T. Bioavailability of resveratrol. Ann N Y Acad Sci. 2011 Jan;1215:9-15. DOI: 10.1111/j.1749-6632.2010.05842.x You should therefore consider supplements of trans Resveratrol extracted from Japanese Knotwood.
Quercetin is a flavonoid that can be found in broccoli, buckwheat, onions, apples, plums, cherries and berries. Quercetin seems to be able to bind to the spike protein, reduces inflammation, inhibits clotting and has antiviral properties. It also helps to inhibit monoamine oxidase, and thus increasing neurotransmitters like serotonin, noradrenaline and dopamine, which helps a lot for your mood. It should be mentioned that high doses of quercetin are able to deplete glutathione levels, which could result in a pro inflammatory effect, so be cautious about proper dosage.16)Chirumbolo S. The role of quercetin, flavonols and flavones in modulating inflammatory cell function. Inflamm Allergy Drug Targets. 2010 Sep;9(4):263-85. DOI: 10.2174/187152810793358741
Hermel M, Sweeney M, Ni YM, Bonakdar R, Triffon D, Suhar C, Mehta S, Dalhoumi S, Gray J. Natural Supplements for COVID19-Background, Rationale, and Clinical Trials. J Evid Based Integr Med. 2021 Jan-Dec;26:2515690X211036875. doi: 10.1177/2515690X211036875 For Long COVID patients it is recommended to supplement 250mg of quercetin daily, together with ingesting the natural sources to maximize the benefits.
Luteolin is acting in about the same lines and is supposed to penetrate better in the brain than quercetin. It was studied already in Alzheimers disease and reduces neuroinflammation and cognitive disfunction. Both quercetin and luteolin are difficult to absorb, but are better available when combined with olive pomace oil.17)Theoharides TC, Cholevas C, Polyzoidis K, Politis A. Long-COVID syndrome-associated brain fog and chemofog: Luteolin to the rescue. Biofactors. 2021 Mar;47(2):232-241. doi: 10.1002/biof.1726 Dietary sources of luteolin include celery, broccoli, green pepper, carrots, olive oil, parsley, thyme, peppermint and oregano.
Vitamin C has many benefits for the immune system. It can regulate the overproduction of histamine by the mast cells. You can supplement with 1,000 mg of vitamin C 2 to 3 times daily. Prolonged high doses can though provoke the development of kidney stones, and should be limited to a few weeks.
Coenzyme Q10 will help to improve mitochondrial function. In patients having chronic fatigue syndrome it was shown that Coenzyme Q10 as well as NADH was low. In a study it was shown that supplementing with 200mg of Coenzyme Q10 and 20mg NADH daily, a substantial improvement in fatigue and the corresponding biomarkers of the energy cycle could be achieved.18)Castro-Marrero J, et.al. Does oral coenzyme Q10 plus NADH supplementation improve fatigue and biochemical parameters in chronic fatigue syndrome? Antioxid Redox Signal. 2015 Mar 10;22(8):679-85 doi: 10.1089/ars.2014.6181
L-Carnitine is an enzyme that helps the body to transform fat into energy. It is important for heart and brain function, muscle movement and many other body processes. Supplementing with 300mg of L-Carnitine daily may help with overcoming fatigue.
A mitochondrial energy optimizer formula, including pyrroloquinoline quinone (PQQ) can be used to strengthen the mitochondria and increase energy levels.
COVID-19 can wreak havoc on your microbiome, which is essential for proper immune function. A study showed that a number of important gut bacteria remained low after a SARS-Cov2 infection for the entire 30 day period of the study.19)Yeoh YK, Zuo T, Lui GC, et al. Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19. Gut 2021;70:698-706. http://doi.org/10.1136/gutjnl-2020-323020 Eating yoghurt (can be plant based), sauerkraut, kefir and other fermented products can help to improve the microbiome, and a high fiber diet helps to nourish your microbiome, but in many cases a prebiotic and probiotic regimen would be indicated to restore proper gut health.
Melatonin is a hormone produced by our body to regulate the sleep/wake cycle. It has also anti-inflammatory and antioxidant properties and supports the gut lining, thus strengthening the immune system. To help regulate the sleep/wake cycle, a supplementation of 1mg at bedtime would be sufficient. If you want to maximize the other benefits, you can gradually increase dosage as tolerated without interfering with sleep, until you reach the maximum dosage of 8mg per day, and preferably a slow-release supplementation should be used.
Vitamin D is essential for proper immune function. Besides strengthening immunity, it also regulates many immune functions in case of allergic overreactions. We did already an article about the importance of Vitamin D to protect and treat COVID-19. Be sure to make regular blood tests and try to maintain a level of 60 to 80 ng/mL in your blood. The FLCCC Alliance has a table which dosage should be used if levels are low. For a maintenance you should supplement with about 5.000 IU per day for normal weight persons, and 10,000 to 25,000 IU depending on obesity levels.
Hydrotherapy
Application of hot and cold water in the form of hydrotherapy treatment is a powerful way to improve circulation. Especially effective will be treatments where hot and cold water are used alternately. They have also a strong immune boosting effect, that can be beneficial in long COVID treatment. There are two options that can be very helpful for improving microcirculation in relation to long COVID.
Contrast Foot Bath
In this treatment, the feet are immersed alternately in a bucket of hot and cold water. The feet have a much higher circulation than other body parts, and are capable in modulating the circulation in the rest of the body.
Start out with the hot water bucket for 3 minutes, then change to the cold water bucket with ice cubes for 1 minute. During this time, have a helper add some hot water to the other bucket in order to increase the temperature gradually, as much as tolerated. Return to the hot water, doing some 5 to 6 cycles, always finishing with cold.
Diabetics and people with impaired sensibility or impaired circulation need to be avoid extremes in temperature in order to avoid burning. Dry off the feet, use some slippers in order to avoid touching the cold floor, and rest for about 30 minutes to potentialize the effect of the treatment.
Contrast Shower
With this treatment you will try to expose the maximum possible area of your skin to the hot to cold change. Start out with 3 minutes of a hot shower, as hot as you can easily tolerate. Then make a brisk switch to cold for 30 seconds to 1 minute. Make 3 cycles, finishing off again with the cold. Dry off and rest for about 40 minutes to potentialize the effect of the treatment.

Herbs
There are plenty of herbs that can give some support in a long COVID treatment protocol. They will have different functions and should be used on an individual basis as needed, but we will mention a few possible options. If you take medications, be sure to check with your doctor about possible interactions.
Astragalus and Chinese skullcap (Scutellaria baicalensis) can aid ACE-2 in some of its functions. We have already said that ACE-2 is inhibited by the SARS-Cov2 virus.
Siberian Ginseng can help to stimulate immunity and reduce inflammation. By enhancing mitochondrial activity, it will be a powerful ally to combat fatigue. It also helps to increase focus and enhance deep sleep.
Ginger and Boswellia have inflammatory balancing actions.
Baical Scullcap (Scutellaria baicalensis) may help also to support ACE-2 in its function. It is an excellent herb for stabilizing mast cells, thus balancing the immune system. The anti-inflammatory effect may lower the risk for clots.
Ginkgo Biloba and Bilberry (Vaccinium myrtillus) have a tonic effect and are beneficial in treating fatigue. Ginkgo has also anti-inflammatory properties and can improve microvascular circulation. It reduces the inflammatory cytokine Interleukin 6, which seems to play an important factor in developing long COVID.20)Kappelmann N, Dantzer R, Khandaker GM. Interleukin-6 as potential mediator of long-term neuropsychiatric symptoms of COVID-19. Psychoneuroendocrinology. 2021 Sep;131:105295. DOI: 10.1016/j.psyneuen.2021.105295
Hawthorn (Crataegus monogyna) can help to repair damage to the inner layer of the blood vessels called endothelium. It can help also to improve cognitive function and regulate the autonomic nervous system for example in case of palpitations (of course after seeing your heart specialist to rule out another cause). Hawthorn may help also with mitochondrial energy production.
There are of course many options of herbs that can find use in long COVID treatment, but this is a selection of some interesting options to choose from.21)Hentschel N. Natural treatments for long covid. Your Remedy Naturopathy, June 30, 2022
Important Lifestyle Measures
Intermittent fasting can help to stimulate phagocytosis, which eliminates damaged cells and makes room for new cells. It helps also to stimulate mitophagy, which is the selective degradation of damaged mitochondria. This is probably one of the best ways to deal with mitochondrial damage caused by COVID-19 in order to recuperate from fatigue. My preferred way to implement intermittent fasting is to skip supper. Read more about the subject in our article about autophagy.

Spermidine and resveratrol are two substances that can still augment the efficacy of autophagy in intermittent fasting. Natural sources of spermidine are wheatgerm, mushrooms, grapefruit, apples and mango. Especially wheatgerm supplements can provide a good spermidine dose. We already spoke about resveratrol supplementation, which should be definitely considered in combination with intermittent fasting.
Proper hydration is essential for many reasons. Considering that about 70% of the body is made out of water, it is easy to understand that dehydration can quickly lead to fatigue and headaches. It is essential for good circulation and even helps your immune system. Quite obviously, good hydration is primordial in the recovery from long COVID. And as a saying goes, you need 5 glasses a day to survive, 8 glasses to do well and 10 glasses to thrive!
Quality sleep is essential for body repair and proper mental functioning. It can contribute much to a better recovery. Unfortunately, many who are suffering from long COVID also struggle to get quality sleep. It is important to go to bed at regular times, ideally somewhere around 9PM and allow at least for 8 hours of sleep. A tranquil environment and a warm bath may help to prepare the mind for a good night´s sleep. Avoid alcohol and caffeine in any form, including green tea. If needed, some herbs like valerian or passion flower can help to fall asleep easier. Melatonin can also be helpful and has the above mentioned additional benefits. Getting at least 30 minutes of sunshine during the day is essential for optimal melatonin levels as well.

If you are suffering from severe fatigue, you may need some extra resting periods during the day. You will probably do better on frequent short rest periods than on fewer longer ones. Break up your tasks into smaller chunks, so that you can motivate you to do another chunk and get a short rest afterwards. Consider the best time for certain activities based on your energy levels.
In case of chronic fatigue, proper pacing is essential. You need to consider that any physical or mental activity will need a certain amount of energy, which you need to manage very carefully. You need to get a feeling every morning how are your energy levels this day, and plan your activity accordingly. Short activities combined with proper rest will help you for better recovery. Try to vary between physical and mental activities, and get your family on board to give you support whenever needed.22)Shepherd C. LONG COVID AND ME/CFS. ME Association, April 2021
Exercise can be an important tool to build up your strength, but you need to be very cautious to not over-exert yourself. Exhaustion can worsen your symptoms and set you back in your recovery. Some people have an alternating pattern of good days and worse days. Doing too much activity on a good day may lead to exacerbation of fatigue and other symptoms on the following day.
Having said that, you should include appropriate exercise in your recovery routine. Start with a short walk and increase the exercise time slowly, as long as you avoid over exertion. If you are improving well, you can start including swimming in a warm pool, slow jogging or gentle cycling. Be sure to monitor your heart rate during those activities and stay below 110 beats per minute, until you show clear signs of improvement.
It is clear that stress can be quite detrimental when you are suffering from severe fatigue, brain fog or any similar symptoms. It is something that upsets our system, robs us energy and can still add to the many symptoms we may already feel. Be sure to do proper planning to avoid stress whenever you can. Cut down some of your responsibilities and give yourself time to recover, before you go back to taking on your full plate of commitments again. If you need some tips on how to control your stress, check out the 10 Minute Guide for Stress Management in order to understand how to deal with stress with an all-inclusive approach.
And last but not least, be sure to be grateful. The habit of gratefulness can do so much to improve your outlook on life and speed up recovery from whatever condition you are facing. After having done what you can, be grateful for the little improvements you are feeling day by day, week by week. Be grateful for everything you have, and be grateful for every day of life that your Creator is giving to you.
We have a special opportunity just for you. If you want to receive practical and up to date advice on how to implement an immunity-boosting lifestyle, simply join the Coronavirus Immunity Challenge and prepare yourself to face the pandemic with a bullet-proof immune system.
Coronavirus Immunity Challenge

Shop for Supplements
If you purchase through one of these links, companies will pay us a commission, which helps us to continue providing quality content for free.

Stay Always Up to Date
Sign up to our newsletter and stay always informed with news and tips around your health.
Martin Neumann was trained for Lifestyle Interventions in 1998 at Wildwood Lifestyle Center & Hospital. Since then he has lectured in different parts of the world about a healthy lifestyle and natural remedies. He is the founder of the Abundant Health website.
References
| ↑1 | Understanding post-COVID-19 symptoms and long COVID https://www.healthdirect.gov.au/covid-19/post-covid-symptoms-long-covid Long COVID or Post-COVID Conditions https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html |
|---|---|
| ↑2 | Klein J. et.al. Distinguishing features of Long COVID identified through immune profiling https://doi.org/10.1101/2022.08.09.22278592 |
| ↑3 | Miranda D. et.al. Long COVID-19 syndrome: a 14-months longitudinal study during the two first epidemic peaks in Southeast Brazil. Transactions of The Royal Society of Tropical Medicine and Hygiene, Volume 116, Issue 11, November 2022, Pages 1007–1014, https://doi.org/10.1093/trstmh/trac030 |
| ↑4 | Bach K. New data shows long Covid is keeping as many as 4 million people out of work. https://www.brookings.edu/research/new-data-shows-long-covid-is-keeping-as-many-as-4-million-people-out-of-work/ |
| ↑5 | Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK: 3 November 2022 https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/3november2022 |
| ↑6 | So hoch ist Ihr Long-Covid-Risiko, wenn Sie sich jetzt infizieren Focus 31.10.2022 |
| ↑7 | Natarajan A, et.al. Gastrointestinal symptoms and fecal shedding of SARS-CoV-2 RNA suggest prolonged gastrointestinal infection. Med (N Y). 2022 Jun 10;3(6):371-387.e9. doi: 10.1016/j.medj.2022.04.001. |
| ↑8 | Mo Perry. How to Treat Long-Haul COVID. Experience Life |
| ↑9 | Shaffer L. Lots of long COVID treatment leads, but few are proven. https://doi.org/10.1073/pnas.2213524119 |
| ↑10 | E Pretorius , Combined triple treatment of fibrin amyloid microclots and platelet pathology in individuals with Long COVID/Post-Acute Sequelae of COVID-19 (PASC) can resolve their persistent symptoms. https://doi.org/10.21203/rs.3.rs-1205453/v1 |
| ↑11 | Weinstock LB, et.al. Mast cell activation symptoms are prevalent in Long-COVID. Int J Infect Dis. 2021 Nov;112:217-226 doi: 10.1016/j.ijid.2021.09.043 |
| ↑12 | Astin R. et.al. Long COVID: mechanisms, risk factors and recovery. https://doi.org/10.1113/EP090802 |
| ↑13 | Naureen Z et.al. Proposal of a food supplement for the management of post-COVID syndrome. European Review for Medical and Pharmacological Sciences, 2021; 25 (1 Suppl): 67-73 |
| ↑14 | Moriya J, Chen R, Yamakawa J, Sasaki K, Ishigaki Y, Takahashi T. Resveratrol improves hippocampal atrophy in chronic fatigue mice by enhancing neurogenesis and inhibiting apoptosis of granular cells. Biol Pharm Bull. 2011;34(3):354-9. DOI: 10.1248/bpb.34.354 Mo Perry. How to Treat Long-Haul COVID. Experience Life |
| ↑15 | Walle T. Bioavailability of resveratrol. Ann N Y Acad Sci. 2011 Jan;1215:9-15. DOI: 10.1111/j.1749-6632.2010.05842.x |
| ↑16 | Chirumbolo S. The role of quercetin, flavonols and flavones in modulating inflammatory cell function. Inflamm Allergy Drug Targets. 2010 Sep;9(4):263-85. DOI: 10.2174/187152810793358741 Hermel M, Sweeney M, Ni YM, Bonakdar R, Triffon D, Suhar C, Mehta S, Dalhoumi S, Gray J. Natural Supplements for COVID19-Background, Rationale, and Clinical Trials. J Evid Based Integr Med. 2021 Jan-Dec;26:2515690X211036875. doi: 10.1177/2515690X211036875 |
| ↑17 | Theoharides TC, Cholevas C, Polyzoidis K, Politis A. Long-COVID syndrome-associated brain fog and chemofog: Luteolin to the rescue. Biofactors. 2021 Mar;47(2):232-241. doi: 10.1002/biof.1726 |
| ↑18 | Castro-Marrero J, et.al. Does oral coenzyme Q10 plus NADH supplementation improve fatigue and biochemical parameters in chronic fatigue syndrome? Antioxid Redox Signal. 2015 Mar 10;22(8):679-85 doi: 10.1089/ars.2014.6181 |
| ↑19 | Yeoh YK, Zuo T, Lui GC, et al. Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19. Gut 2021;70:698-706. http://doi.org/10.1136/gutjnl-2020-323020 |
| ↑20 | Kappelmann N, Dantzer R, Khandaker GM. Interleukin-6 as potential mediator of long-term neuropsychiatric symptoms of COVID-19. Psychoneuroendocrinology. 2021 Sep;131:105295. DOI: 10.1016/j.psyneuen.2021.105295 |
| ↑21 | Hentschel N. Natural treatments for long covid. Your Remedy Naturopathy, June 30, 2022 |
| ↑22 | Shepherd C. LONG COVID AND ME/CFS. ME Association, April 2021 |









Leave a Reply